Historical Perspectives On Contemporary Issues
Trust in Science: Vaccines
A forum held at the American Philosophical Society on January 29, 2019, and continued online here.
2019 Albert M. Greenfield Forum in the History of Science
Join us to examine vaccine skepticism—in contemporary America, historically, and in the clinic. What are the historical roots of resistance to vaccination? What does the data about contemporary attitudes show? How do these attitudes relate to changing social, economic and political contexts? How do these issues play out in the relationship between a doctor and a patient? Three experts will share their research and experience on these questions, and lead our discussion.
"Trust in Science: Vaccines" is the first event in a series inspired by Perceptions of Science in America, a report from the Public Face of Science Initiative at the American Academy of Arts and Sciences. Two more events will cover trust in science through evolution and climate change. This series is presented by the Consortium for History of Science, Technology and Medicine.
Featuring
 Jeffrey Baker
Duke University
Jeffrey Baker
Duke University
 Elena Conis
University of California, Berkeley
Elena Conis
University of California, Berkeley
Elena Conis is Associate Professor at the University of California, in the Graduate School of Journalism, the Center for Science, Technology, Medicine and Society, and the Program in Media Studies--as well as the Department of Anthropology, History and Medicine at the University of California, San Francisco. Her book, Vaccine Nation: America’s Changing Relationship with Immunization, won the Arthur J. Viseltear Award for contributions to the history of public health from the American Public Health Association in 2015.
 Robert M. Hauser
American Philosophical Society
Robert M. Hauser
American Philosophical Society
Robert M. Hauser is Executive Officer of the American Philosophical Society and is part of the American Academy of Arts and Sciences Public Face of Science steering committee.
 Erica Kimmerling
American Academy of Arts and Sciences
Erica Kimmerling
American Academy of Arts and Sciences
Erica Kimmerling is Senior Advisor for Science Engagement Policy and Partnerships at the Association of Science and Technology Centers in Washington, D.C. Prior to this, Erica was the Hellman Fellow in Science and Technology Policy at the American Academy of Arts and Sciences where she worked on the Public Face of Science project.
Mailman School of Public Health, Columbia University
James Colgrove conducts research on the relationship between individual rights and the collective well-being, and the process through which public health policies have been mediated in American history.
The three presenters do an excellent job of highlighting the sociopolitical, legal, and ethical challenges surrounding trust in vaccines. Their talks illuminate the complexity of this issue and the need to grapple not just with questions of trust, but with deeply rooted beliefs about communal rights and responsibilities in a pluralistic and closely interconnected society. I would like to make three observations prompted by the insights provided in these presentations.
Mailman School of Public Health, Columbia University
The three presenters do an excellent job of highlighting the sociopolitical, legal, and ethical challenges surrounding trust in vaccines. Their talks illuminate the complexity of this issue and the need to grapple not just with questions of trust, but with deeply rooted beliefs about communal rights and responsibilities in a pluralistic and closely interconnected society. I would like to make three observations prompted by the insights provided in these presentations.
First, the talks reminded me once again that the law is one of the most effective tools in the public health toolkit, albeit one that must be used carefully and with attention to political context. As I write this in March 2019, legislators in Arizona and Washington are debating the issue of exemptions to school immunization laws; opponents of mandatory vaccination are vociferously making their views known and in some cases gaining the ears of sympathetic lawmakers. As Elena Conis notes, such debates are as old as vaccination itself. More than 200 years since Massachusetts enacted the first compulsory vaccination law, school-based requirements are a critically important way of maintaining herd immunity, and a large empirical literature has demonstrated the effectiveness of these laws. At the same time, they have been a flashpoint for court cases and legislative battles throughout history. Opposition to compulsory vaccination defies easy ideological pigeonholing. This is an issue where opposite ends of the political spectrum—the ACLU left and the Tea Party right—can find common cause, and much has been made of the potential for backlash in the aggressive use of law, and the counterproductive effects of a mandate that lacks public support. On the other hand, it is useful to remember that school immunization laws do enjoy wide support. Events in California since 2015 provide an encouraging illustration of this. In the aftermath of the Disneyland measles outbreak, the state eliminated nonmedical (religious and philosophical) exemptions to its school immunization law. Opponents reacted with outrage and sought to overturn the new law via referendum, but that effort failed to gain enough signatures to qualify for the ballot, as did an attempt to recall the state senator who authored the bill eliminating nonmedical exemptions. It is also worth remembering that the two other states that have no nonmedical exemptions, Mississippi and West Virginia, have successfully maintained these laws on the books for decades. These states’ high rates of immunization coverage attest both to the effectiveness of a strict law and the possibility of administering such a law without engendering political blowback.
Second, the heterogeneity of concerns about vaccination, which the panelists very effectively convey, will require broadly multidisciplinary research efforts in order to develop effective policies and practices to build trust. Thanks in part to a growing body of empirical research, we have a fairly nuanced understanding of the motivations that are grouped under the umbrella of “anti-vaccination,” a term, as Jeff Baker reminds us, that encompasses a wide spectrum of attitudes and beliefs. This term, as well as the slangy short-hand “anti-vaxx,” which has come into fashion in popular media commentary in the last few years, has the unfortunate effect of obscuring meaningful differences in the underlying motivations of those who decline vaccines. Although our understanding of what motivates people to decline vaccination for themselves and their children has grown considerably in the past two decades, there is a long way to go to fully understanding what drives this behavior, and an even longer way to go to translating this understanding into effective interventions. Just as the panel brought to bear analyses informed by history, survey research, quantitative sociology, and clinical experience, the challenge of building trust in vaccines will require public health researchers and practitioners to draw upon methods and concepts from a variety of social and behavioral sciences. In-depth qualitative research and ethnographic approaches, exemplified by the work of scholars such as Jennifer Reich, Emily Martin, and Elisa Sobo; theoretical and empirical guidance from health communication researchers such as Jeff Niederdeppe and Vish Viswanath; and insights from behavioral economists such as Brendan Nyhan can give us a more sophisticated and nuanced understanding and better tools to tackle the challenge of building and maintaining trust.
A final insight I took away from this panel is that the difficulty of maintaining trust in vaccines mirrors the central challenge facing the public health enterprise as a whole: how to help the lay public understand and appreciate the value of prevention. As Alfred Sommer, former dean of the Johns Hopkins Bloomberg School of Public Health, has argued, public health is “an invisible health system that promises, as an outcome, abstract non-events.” The freedom our country enjoys from formerly widespread vaccine-preventable diseases is a paradigmatic example of the “abstract non-event.” As noted in the roundtable discussion, people do not see the cases of polio or smallpox that no longer occur; these “non-cases” lack the psychological salience that would help to engender public trust in the measures that eliminated them. By a similar token, the public health profession has been responsible—invisibly—for millions of lives saved though preventive measures too numerous to name, including limits on environmental pollution, workplace safety regulations, safety features in automobiles, and surveillance systems that enable us to track and respond to disease incidence and prevalence. How does a field whose benefits are “negative” or inapparent achieve the social, political, and economic support this work requires? In at least one respect, immunization is in a better position than some other “invisible” public health measures because of the role that clinicians play in implementing it. The high levels of trust people continue to report in their own primary care provider, no matter how much dissatisfaction they may feel about the health care system in the abstract, may give us reason for optimism.
Department of International Health,Bloomberg School of Public Health, Johns Hopkins University
Neal Halsey conducts research and teaches toward the prevention of infectious disease with the safest vaccines possible. He works with the Johns Hopkins Vaccine Initiative, the Center for Global Health, and the Institute for Vaccine Safety.
The Consortium for History of Science, Technology and Medicine meeting on "Trust in Science: Vaccines." held January 29, 2019 provided a superb review of the social, cultural and historical contexts of skepticism about vaccines. Vaccine hesitancy and refusal has recently gained widespread attention amid measles outbreaks in multiple U.S. states, Europe and other countries that are largely due to vaccine hesitancy and/or refusal(1,2). Everyone interested in the problem of vaccine acceptance and the unnecessary suffering from preventable infectious diseases should listen to the webcast.
This commentary is coauthored with Daniel Salmon
See more...Department of International Health,Bloomberg School of Public Health, Johns Hopkins University
This commentary is coauthored with Daniel Salmon
The Consortium for History of Science, Technology and Medicine meeting on "Trust in Science: Vaccines." held January 29, 2019 provided a superb review of the social, cultural and historical contexts of skepticism about vaccines. Vaccine hesitancy and refusal has recently gained widespread attention amid measles outbreaks in multiple U.S. states, Europe and other countries that are largely due to vaccine hesitancy and/or refusal(1,2). Everyone interested in the problem of vaccine acceptance and the unnecessary suffering from preventable infectious diseases should listen to the webcast.
Erica Kemmerling from the American Academy of Arts and Science provided intriguing data showing decreasing trust in banks and financial institutions, Congress, and the press in recent years, but the percentage (about 40%) of US adults reporting a “great deal” of confidence in the scientific community has remained very stable. Also, more than 70% of people say that the benefits of scientific research outweigh the harmful results. Confidence in the leaders of the scientific community varies by race, gender, age, geographical region, education, and political affiliation. Those of us who believe personal and political decisions should be made on the basis of good science would like to see a higher percentage of the general public expressing high levels of confidence in scientific leaders who make important decisions that affect our lives and those of our children. Clearly, there is more that can and should be done to educate the public about the value of science in decision making, including acceptance of recommended vaccines.
Dr. Elena Conis from the Center for Science, Technology, Medicine, and Society and the University of California, Berkeley, provides an historic review of trust in vaccines. Over the past 50 years we have seen great growth in the potential of vaccines to prevent diseases, but also increased opposition to mandates requiring recommended vaccines for children. Public health authorities have played an important role in approving, providing and promoting new vaccines, as well as assessing safety. Public perceptions have changed from high enthusiasm for vaccines in the 1950s and 1960s when polio, measles and other vaccines were first introduced, to a shift in recent years to questioning the need for and safety of some vaccines. These changes have paralleled decreasing trust in government. Dr. Conis concludes by stating “Trust in vaccination goes hand in hand with trust in government”.
Dr. Jeffrey Baker from Duke University School of Medicine provides a history of trust in vaccines from a clinician’s perspective. Changing parental expectations include old-style medical paternalism giving way to patient empowerment and choice, increasing popularity of “natural” mothering, and consumerism increasingly being promoted in medicine. The result, as described by Dr. Baker, was the perfect storm whereas the “autism epidemic” met vaccine skepticism. Dr. Baker argues that vaccine hesitancy – like autism – is a spectrum whereas a few might fit the stereotype of extreme distrust and conspiracy theories, but far more people find themselves honestly worried. People want to make choices in according to their values which vary tremendously between people. No “one size fits all” is sufficient to address the varying concerns and values that clinicians encounter. Trust in doctors is critically important for patient decision making, particularly around vaccines.
Dr. Baker and the great majority of physicians and public health personnel involved in vaccines and vaccine programs were unaware of the amount of mercury in thimerosal containing vaccines in 1999 when the FDA review revealed that the potential exposure to ethylmercury among infants to be more than the Environmental Protection Agency considered to be safe based on guidelines for exposure to methyl mercury. The guidelines for methyl mercury were based on low level chronic exposure through diet rather than vaccine exposure to ethyl mercury which were bolus exposures through injection. The active efforts to encourage reduction or elimination of thimerosal in vaccines given to infants was necessary as a precautionary measure because of the uncertainties regarding differences in toxicity between ethyl and methyl mercury. Imagine the public backlash that would have occurred if action was not taken to decrease exposure for infants. The loss in public trust in vaccines, government, and the medical profession would have been very large.
Maintaining trust in vaccines, public health authorities, and health care providers will require a multi-faceted effort. We can improve the public’s understanding of science by increasing efforts to teach scientific decision making at all levels of education. Understanding science and how decision are made overcomes the fallacy of “post hoc ergo propter hoc” or “after this, therefore because of this”. The public needs to know more about the science that goes into the development and evaluation of vaccines. Basic information about vaccines and how they benefit individuals and communities should be included in the curriculum for children, beginning in elementary school and continuing through adolescence.
Many vaccines have been developed with support from the National Institutes of Health which uses a rigorous peer review process for funding studies that have contributed to the development of many of the vaccines available today. The Food and Drug Administration (FDA) conducts in-depth reviews of applications for licensure by manufacturers. Clinical trials are required to characterize efficacy and safety, and proof that the benefits outweigh the potential risks. Also, there is an underappreciation for the careful reviews of evidence that goes into decision making recommendations for the use of approved vaccines coordinated by the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices (ACIP), with input from the American Academy of Pediatrics, the American Academy of Family Physicians, the American College of Physicians, and many other professional societies and organizations. Anyone can now observe these decision making processes by watching the live webcasts of the FDA advisory committee meetings and the ACIP. After licensure the FDA and the CDC monitor vaccines for safety (3).
Fortunately, only 1-2% of parents in the United States are ideologically opposed to vaccines. However, 7 in 10 parents express concerns about the safety of vaccines and 1 of 3 parents express concerns about autism, vaccine ingredients or the number of vaccines given at one visit or the first two months of life(4). Realizing the full potential of vaccines to prevent disability and save lives requires ensuring that this substantial group of concerned, but not ideologically opposed, parents accept timely vaccination for their children. It will require a continuing effort on the part of scientists, clinicians and public health authorities to maintain trust in vaccines to effectively control and possibly eradicate vaccine preventable diseases.
- Centers for Disease Control and Prevention https://www.cdc.gov/measles/cases-outbreaks.html
- World Health Organization: http://www.euro.who.int/en/media-centre/sections/press-releases/2019/measles-in-europe-record-number-of-both-sick-and-immunized
- Department of Health and Human Services. https://www.hsdl.org/?view&did=6793
- Kennedy A, Lavail K, Nowak G, Basket M, Landry S. Confidence about vaccines in the United States: understanding parents perceptions. Health Aff. 2011 Jun; 30(6): 1151-9.
Department of Philosophy, Oakland University
Mark Navin specializes in applied ethics, bioethics, and social and political philosophy.
I am delighted to contribute to the conversation—on Trust in Science: Vaccines—kicked off by informative and insightful talks from Erica Kimmerling, Elena Conis, and Jeffrey Baker. I want to reflect on how these speakers’ contributions can inform our assessment of the kinds of arguments people make in their attempts to understand and respond to vaccine refusal. Vaccine advocates commonly criticize the arguments offered by vaccine refusers. I think vaccine advocates can protect their own cognitive hygiene by holding themselves to similarly high standards of reasoning.
Department of Philosophy, Oakland University
I am delighted to contribute to the conversation—on Trust in Science: Vaccines—kicked off by informative and insightful talks from Erica Kimmerling, Elena Conis, and Jeffrey Baker. I want to reflect on how these speakers’ contributions can inform our assessment of the kinds of arguments people make in their attempts to understand and respond to vaccine refusal. Vaccine advocates commonly criticize the arguments offered by vaccine refusers. I think vaccine advocates can protect their own cognitive hygiene by holding themselves to similarly high standards of reasoning.
Here is a bad argument commonly offered by vaccine refusers:
Premise: I know a child who experienced an injury soon after being vaccinated.
Conclusion: Therefore, a vaccine (or vaccines) caused that child’s injury.
We may have reason to doubt the premise. Perhaps this child never had the relevant injury, or perhaps the injury arose before or long after vaccination? But even if the premise gets the facts right, the conclusion does not follow. This argument commits a classic fallacy: post hoc ergo propter hoc (after this, therefore resulting from it), i.e. when a person infers a causal relationship between two phenomena because of their close temporal proximity.
Advocates of vaccination are right to criticize the bad reasoning offered by vaccine refusers. But they could sometimes be more vigilant about their own tendencies to engage in sloppy reasoning. In the five arguments I discuss, below, I say something about where and why I think this bad reasoning can happen. I generally assume the premise of each argument is true, since my point is that our reasoning can go astray even when we get the facts right. But if anyone wants to debate the premises, I’d be happy to do that, too.
Fallacies about Understanding Vaccine Refusal
Here are three ways in which we can reason badly about the nature of vaccine refusal.
1. Anti-Science Fallacy
Premise: Vaccine refusers reject scientific consensus views.
Conclusion: Therefore, vaccine refusers are anti-science.
There is an overwhelming scientific consensus that vaccines are safe, with very rare serious side effects. Many vaccine refusers believe that vaccines are not safe. Therefore, many vaccine refusers reject a scientific consensus view. But does it follow that vaccine refusers are anti-science?
First, we should be skeptical about whether vaccine refusers know the scientific consensus about vaccine safety. According to the AAAS report reviewed by Erica Kimmerling, only 55% of Americans surveyed agreed that “Almost All” medical scientists believe the MMR vaccine is safe. So, even if vaccine refusers are rejecting consensus claims, they may not believe that is what they are doing. Second, even if vaccine refusers knew they were rejecting a consensus scientific view about MMR safety, it wouldn’t follow that they reject science generally, or that they participate in other contemporary forms of organized science denialism. Indeed, research (including the research the AAAS report draws from) shows there is no significant overlap between people who reject the science of vaccines, evolutionary biology, GMO crops, and anthropogenic climate change.
The Anti-Science Fallacy goes wrong because it attributes intentions, beliefs, and identities to vaccine refusers, in the absence of sufficient evidence for doing so. It can be tempting to conceive of conflicts over science-informed policies as battles between pro-science and anti-science tribes, but this kind of Manichaeism obscures more than it illuminates.
2. Race and Trust Fallacy
Premise: Vaccine refusers are more likely to be white than black.
Conclusion: Therefore, white people have less trust in vaccines than black people do.
In the United States, white people are overrepresented among applicants for nonmedical exemptions to school or daycare immunization mandates. (Applicants for nonmedical exemptions are often our best proxy for vaccine refusers, since it can be otherwise difficult to distinguish people who are unvaccinated by choice from those who are unvaccinated because of poor access to vaccines.) We also know that trust in vaccines is strongly associated with a decision to vaccinate. So, we might conclude that white people are less trusting of vaccines than black people are. In her discussion of the AAAS report, Perceptions of Science in America, Kimmerling notes that there are race-based differences in the trust people Americans in vaccines, but this relationship is the opposite of what the Race and Trust Fallacy suggests: The Pew Research Center Report (that the AAAS report draws from) found that black Americans were less likely that white Americans to trust in the safety of vaccines.
The Race and Trust Fallacy goes wrong because it presumes too tight a causal connection between trust in vaccines and vaccine compliance. Many black Americans comply with vaccine mandates even though they do not trust that vaccines are safe. ‘Untrusting compliance’ surely has many explanations, as medical sociologists and others have documented. Our recognition of this phenomenon should incline us to cast wider nets in our efforts to identify the factors that contribute to vaccination decisions.
3. Safety Causes Trust Fallacy
Premise: Vaccines are safe.
Conclusion: Therefore, vaccine refusers should trust government statements that vaccines are safe.
Vaccine refusers often distrust statements about the safety of vaccines offered by the government, physicians, and scientific researchers. Among other reasons, this is because vaccine refusers believe there is good evidence—from historical and contemporary experience—to doubt the veracity of the claims made by these institutions and individuals, especially about medical safety. (Both Elena Conis and Jeffrey Baker identify some of the relevant historical evidence.)
In response to these worries about trust, vaccine advocates sometimes object “But vaccines are safe!” Usually this argument (from safety to trust) is made only implicitly, as when my Twitter feed recently exploded with retweets about a new paper that showed an absence of a link between vaccination and autism, and when those retweets were headed by comments like “Do you believe us now, vaccine refusers?” From the point of view of an individual physician, scientist, or public health official, a new scientific paper that affirms a consensus view likely provides additional evidence for that view, and therefore lends credence to the other individuals and institutions who have expressed that view. But from the point of view of many vaccine refusers, pro-vaccination individuals and institutions can seem like a monolithic untrustworthy voice. When that voice repeats itself—saying yet again that “vaccines are safe”—it is naïve to think that this kind of repetition would increase the credence that vaccine refusers grant to vaccine advocates.
The Safety Causes Trust Fallacy goes wrong because it equivocates between truth and trust, and because it is insensitive to the broad skepticism with which many vaccine refusers treat the individuals and institutions who promote vaccines. As Babak Ashrafi notes in his introductory remarks, we would do well to attend to the differences between trust and truth, and to the differences between the conditions in which each of these phenomena obtains.
Fallacies about Responding to Vaccine Refusal
Here are two ways in which we can reason badly about how to respond to vaccine refusal.
4. Information Deficit Fallacy
Premise: Vaccine refusers have false beliefs about vaccines.
Conclusion: Therefore, efforts to correct vaccine refusers’ false beliefs will cause them to vaccinate.
Many people have argued that education about immunization should be central to private and public responses to vaccine refusal. This makes intuitive sense. When someone has a false belief, and when their false belief is a cause of a bad behavior, we may reasonably hope to change their behavior by correcting their false belief.
One worry about this kind of argument is that it does not follow from the fact that someone embraces a falsehood about vaccines that this false belief is what motivates them to refuse vaccines. For example, Conis argues in her book (Vaccine Nation, University of Chicago, 2015) that a vaccine refuser who says ‘vaccines cause autism’ may be invoking this claim as a proxy for a set of other (often more difficult to identify) motivations they have for refusing vaccines, including worries about over-medicalization, a commitment to more ‘natural’ ways of life, and the pursuit of hyper-intensive forms of parenting (and parental vigilance). This kind of parent may believe that vaccines cause autism, but that belief is unlikely to be their only (or even their most pressing) objection. Another worry about the Information Deficit Fallacy is that efforts to correct vaccine refusers’ false beliefs may be ineffective or even counter-productive. Even if we could identify a particular false belief that led an individual to refuse vaccines, it does not follow that we could persuade them to abandon that false belief, or that our efforts to do so would result in increased vaccine compliance even if we succeeded in changing a person’s belief.
The Information Deficit Fallacy goes wrong because it assumes that a vaccine refuser’s stated objections are their true motivations, and that correcting falsehoods changes people’s beliefs and behaviors.
5. Analogical Coercion Fallacies
Premise: In other contexts, the state is ethically justified in using coercion to promote the same kinds of goals that vaccines promote.
Conclusion: Therefore, the state is ethically justified in using coercion to promote vaccination.
Many countries, including Australia, France, Italy, and the United States, have recently implemented or revised vaccine mandates. (As Jeffrey Baker and Robert Hauser’s comments may suggest, if pro-vaccination communication in clinical encounters cannot ensure sufficiently high immunization rates, state interventions may be necessary.) It is therefore especially important to determine how best to ethically justify these kinds of policies. Many advocates of increased state coercion for immunization invoke arguments by analogy with other justified uses of state power. For example, they note that it can be legitimate for the state to compel tax payments, criminalize the discharge of weapons in populated areas, and override parental discretion when children need life-saving blood transfusions. This is because the state can force people to make fair contributions to valuable public projects, prevent people from harming third parties, and protect children from parental neglect. These three reasons also count in favor of vaccine mandates. So, it may seem to follow that the state may use coercion to promote vaccination.
In reply, arguments by analogy are only as strong as the relevant similarities between the cases under comparison. But in some cases the relevant values— fairness, harm prevention, and children’s interests—may not provide the same weight for vaccine mandates as they provide for other instances of justified state coercion that promote these values. For example, refusal of MMR when immunization rates are relatively high is not nearly as risky for children as refusing life-saving blood transfusions. In other cases, the values invoked by analogical arguments for vaccine mandates may tell equally (enough) in favor of both vaccine mandates and other coercive policies. But this would not be enough for an ethical justification of vaccine mandates, because other values may tell against vaccine mandates, but not (or not as much) against the analog policy. For example, even though fairness (i.e. a duty not to free-ride on community protection) counts in favor of vaccine mandates, a mandate that keeps unvaccinated children out of school may prevent children from receiving an education, block parents (usually mothers) from entering or remaining in the workforce, and prevent the state from supervising unvaccinated children.
Analogical Coercion Fallacies go wrong because they fail to account for the wide array of values implicated by vaccine mandates, and the ways in which the diverse forms of vaccine mandates implicate those values. The fact that these arguments are fallacies does not mean that vaccine mandates are unjustified, but that additional evidence (and better reasoning!) is necessary.
Conclusion
It’s important to get the facts right when we talk about vaccine refusal. But it’s just as important to reason well. I hope to have made helpful suggestions for how to reason better about vaccine refusal.
Department of Sociology, University of Colorado, Denver
Jennifer Reich is a sociologist whose research has examined how parents come to reject vaccines for their children, in dialog with physicians, complementary healthcare providers, activists, and researchers. She is the author of Calling the Shots: Why Parents Reject Vaccines (NYU Press).
When I began writing about mothers and vaccine refusal in 2014, I would be regularly asked at conferences and by colleagues and students, “How did you know vaccines would become a big issue?” The easy answer, the one of which Elena Conis so eloquently reminds us, is that vaccines have been a big issue since their inception. In fact, vaccine refusal, distrust of government policies that require use of vaccines, and the claims of safety and efficacy are not new.
See more...Department of Sociology, University of Colorado, Denver
When I began writing about mothers and vaccine refusal in 2014, I would be regularly asked at conferences and by colleagues and students, “How did you know vaccines would become a big issue?” The easy answer, the one of which Elena Conis so eloquently reminds us, is that vaccines have been a big issue since their inception. In fact, vaccine refusal, distrust of government policies that require use of vaccines, and the claims of safety and efficacy are not new. Each of these speakers provided an accessible and compelling way to help us situate the current moment of vaccine refusal within larger contexts of history, culture, and political perspectives to think of these old questions in new ways. I am honored to be a part of this forum to discuss this important topic.
Clearly, this topic also has particular cultural resonance today. As we watch increasing numbers of outbreaks of vaccine-preventable diseases and see the US on pace for a record-setting rate of measles infections since the development of the vaccine, the quick and common response—one I hear everywhere I go when discussing vaccine hesitance and refusal—is simply, what is wrong with these people?
When we ask about these people, or those parents, we mostly mean women. As Jeffrey Baker mentioned, Jenny McCarthy is most often invoked as the face of the anti-vaccine movement, despite her recent insistence she is not anti-vaccine, but “pro-safe vaccine.” Virtually whenever she is mentioned, she will be referenced not as a mother or writer, but as a Playboy centerfold. Vaccine refusal is in fact women’s territory. Mothers are most likely to be in charge of making children’s healthcare decisions and they are most likely to feel distrustful of the information they are offered. However, the particularly gendered way that the public dismisses Jenny McCarthy reflects a larger challenge we collectively face in thinking through how we understand mothers who refuse consent to vaccines for their children. The easiest way to understand them is as confused or misguided. At times, they are referenced as “anti-science,” more trusting of google than physicians, or simply ignorant of the diseases vaccines prevent. In my own work, which builds on the work of these panelists and my fellow commentators, I aim to take seriously how women—disproportionately white and college educated—reach the decision to reject some or all vaccines and how they decide to substitute their own judgment for that of Center for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP), the American Academy of Pediatrics (AAP), and other experts.
One way to take seriously the process by which mothers come to reject vaccines is to take seriously the endless, highly scrutinized work of mothering. In fact, women are asked even before they become pregnant to make informed consumer decisions that will protect or optimize their off-spring. They are told to research brands, read labels, prepare healthy food—even when it is laborious, expensive, and time-consuming—breastfeed infants, nurse kids back to health, make education choices that best fit their child’s needs, remain vigilant of potential risks, and ensure children’s success.[i] Mothers with disabled children, as Baker reminds us, often face scrutiny about what they might have done wrong, whether it was during pregnancy or after, to cause this disability. Mothers are culturally held responsible for children’s health and well-being, particularly in societies like in the U.S. that do not ensure adequate support for children’s health, education, and well-being.
The finding presented by Erica Kimmerling suggest provocatively that women were more distrustful of expert claims. Yet, it is worth considering how these experts, disproportionately men, often do not take the insights of women or the hard work of mothering seriously, do not recognize the labor that goes into making decisions for one’s children, and do not always empathize with the scrutiny mothers inescapably face. Both Conis and Baker highlight how the early 1980s and questions about the pertussis component of the DPT vaccine changed vaccine regulation and parents’ perceptions. Part of this history, they note, includes the way this television expose’ created parent networks where none had existed. When the televised special Vaccine Roulette aired in 1982, parents who saw it called NBC and were put in touch with other parents who believed their children had been harmed by the DPT vaccine. In my own research, I heard stories of how some of these parents felt betrayed by the experts they had trusted who assured them vaccines were safe and their subsequent frustration that many doubted their claims that their children had been injured by those vaccines. Baker makes clear there is among experts an unresolved robust disagreement about whether the pertussis component of this live vaccine caused harm. Yet, for the parents whose children died or regressed, there is little uncertainty. Perhaps this reveals parents’ early distrust of science. Yet it also reveals experts’ distrust of parents.
Baker argues compellingly that mothers aim to “make a responsible choice based on their values.” This kind of consumer choice indeed reflects individual values, but it is worth noting that those personal values are not developed in isolation but reflect conversations with family and friends, feedback from other mothers, evaluation from institutions, and often, advice of experts—even if not those who are members of ACIP or AAP. We also must remember that the ability to exercise choice is not equally available to all parents; families have as much choice as they can afford. As Conis reminds us, vaccines, prior to the 1960s, were most available to wealthy families. Legal mandates became a way to ensure greater public funding for vaccines, which in turn could support greater access to vaccines for all children irrespective of family resources. In so doing, those families who value vaccines and want to choose them have the option to gain access. Today, as we are observing in California, medical exemptions are also most available to families with resources and networks to find doctors who are willing to write a letter justifying a medical exemption for a fee.[ii] At other times, vaccine shortages or limits in distribution compromise low income and rural families’ ability to exercise choice. In these ways, consumer choice, even when driven by values, remains unachievable for some.
We have generally asked mothers to listen to experts, but to also become individual judges of what their children most need. We ask them to be vigilant guardians, tireless advocates, and also savvy consumers. We do so in a cultural landscape that sets up healthcare as an individual responsibility—where apps can count steps or calories, websites can list the safest products to buy, watches can provide feedback on the quality of sleep, and one will be bludgeoned daily, whether on social media or from their employer-based health insurance company, with new health promoting lifestyle changes they should aspire to make. We also are watching public health agencies sacrifice advocacy for community-level solutions to large-scale problems in favor of focus on education to lead to individual behavioral change.[iii] Perhaps then, we have set the stage for women aiming to be good mothers to distrust experts and decide for themselves whether they believe vaccines are more beneficial than risky. Said differently, mothers who have claimed many of the promises of the women’s health movement (as Conis highlights)—that expertise could be democratized, that lived experiences matter in healthcare, and that healthcare should feel personalized—are insisting that they are best qualified to decide if the diseases vaccines prevent are worse than the deleterious outcomes they fear vaccines may cause.
This leaves us with an important question of how we should move forward to protect everybody in the community, particularly those who cannot be vaccinated, who are too young or too old to be immunized, or for whom vaccines may not work, while also recognizing the hard work of mothering and the process that leads some mothers to reject vaccines. I am heartened by the comments of Conis and Kimmerling who remind us that for the most part, we have very high levels of trust in science and vaccines and that this has been stable over the past several decades. It is easy to lose sight of this significant accomplishment. As we face hundreds of cases of measles in 2019, we should note how far we are from the 3-4 million cases each year that the U.S. saw prior to the creation of a vaccine.[iv] This is not to suggest that there is no work to do. Rather, we may be better served returning to the broader question of values that inform choice.
In my own research, I spoke with mothers who reject vaccines, but see themselves as good people who value community. They describe themselves as working to eliminate toxins from their environment, promote organic food sources, and connect socially with other mothers. Many expressed feeling hurt by the vitriol they face for opting out of vaccines. This suggests an opportunity moving forward to consider how to best make vaccine participation a part of our larger discussions of community participation and social justice. This may require talking about vaccines as more than simply an individual technology for individual benefit. It may require talking about all the children in the community, even those whose parents lack resources to fully actualize their vision for their children’s future or whose values differ from our own. And it may implicate the rest of us as well as we each could do more to think about the limitations of individualizing parenting and personalizing healthcare into a series of individual consumer choices most available to those with the most resources.
Blum, Linda. 1999. At the Breast: Ideologies of Breastfeeding and Motherhood in the Contemporary United States. Boston: Beacon.
Bowen, Sarah, Joslyn Brenton, and Sinikka Elliott. 2019. Pressure Cooker: Why Home Cooking Won't Solve Our Problems and What We Can Do About It: Oxford University Press.
CDC. Measles History. Centers for Disease Control and Prevention 2018 [cited. Available from https://www.cdc.gov/measles/about/history.html.
MacKendrick, Norah. 2018. Better Safe than Sorry. Precautionary Consumption in Everyday Life. Berkeley: University of California Press.
Mohanty, Salini, Alison M. Buttenheim, Caroline M. Joyce, Amanda C. Howa, Daniel Salmon, and Saad B. Omer. 2019. California’s Senate Bill 277: Local Health Jurisdictions’ Experiences With the Elimination of Nonmedical Vaccine Exemptions. American journal of public health 109 (1):96-101.
Shostak, Sara. 2013. Exposed science: genes, the environment, and the politics of population health: University of California Press.
Waggoner, Miranda. 2017. The Zero Trimester: Pre-Pregnancy Care and the Politics of Reproductive Risk: Univ of California Press.
[i] (MacKendrick 2018; Bowen, Brenton, and Elliott 2019; Blum 1999; Waggoner 2017)
[ii] (Mohanty et al. 2019)
[iii] (Shostak 2013)
[iv] (CDC 2018)
Department of International Health, Bloomberg School of Public Health, Johns Hopkins University
Daniel Salmon's research and practice focus on determining the individual and community risks of vaccine refusal, understanding factors that impact vaccine acceptance, evaluating and improving state laws providing exemptions to school immunization requirements, developing systems and science in vaccine safety, and effective vaccine risk communication.
The Consortium for History of Science, Technology and Medicine meeting on "Trust in Science: Vaccines." held January 29, 2019 provided a superb review of the social, cultural and historical contexts of skepticism about vaccines. Vaccine hesitancy and refusal has recently gained widespread attention amid measles outbreaks in multiple U.S. states, Europe and other countries that are largely due to vaccine hesitancy and/or refusal(1,2). Everyone interested in the problem of vaccine acceptance and the unnecessary suffering from preventable infectious diseases should listen to the webcast.
This commentary is coauthored with Neal Halsey.
See more...Department of International Health, Bloomberg School of Public Health, Johns Hopkins University
This commentary is coauthored with Neal Halsey.
The Consortium for History of Science, Technology and Medicine meeting on "Trust in Science: Vaccines." held January 29, 2019 provided a superb review of the social, cultural and historical contexts of skepticism about vaccines. Vaccine hesitancy and refusal has recently gained widespread attention amid measles outbreaks in multiple U.S. states, Europe and other countries that are largely due to vaccine hesitancy and/or refusal(1,2). Everyone interested in the problem of vaccine acceptance and the unnecessary suffering from preventable infectious diseases should listen to the webcast.
Erica Kemmerling from the American Academy of Arts and Science provided intriguing data showing decreasing trust in banks and financial institutions, Congress, and the press in recent years, but the percentage (about 40%) of US adults reporting a “great deal” of confidence in the scientific community has remained very stable. Also, more than 70% of people say that the benefits of scientific research outweigh the harmful results. Confidence in the leaders of the scientific community varies by race, gender, age, geographical region, education, and political affiliation. Those of us who believe personal and political decisions should be made on the basis of good science would like to see a higher percentage of the general public expressing high levels of confidence in scientific leaders who make important decisions that affect our lives and those of our children. Clearly, there is more that can and should be done to educate the public about the value of science in decision making, including acceptance of recommended vaccines.
Dr. Elena Conis from the Center for Science, Technology, Medicine, and Society and the University of California, Berkeley, provides an historic review of trust in vaccines. Over the past 50 years we have seen great growth in the potential of vaccines to prevent diseases, but also increased opposition to mandates requiring recommended vaccines for children. Public health authorities have played an important role in approving, providing and promoting new vaccines, as well as assessing safety. Public perceptions have changed from high enthusiasm for vaccines in the 1950s and 1960s when polio, measles and other vaccines were first introduced, to a shift in recent years to questioning the need for and safety of some vaccines. These changes have paralleled decreasing trust in government. Dr. Conis concludes by stating “Trust in vaccination goes hand in hand with trust in government”.
Dr. Jeffrey Baker from Duke University School of Medicine provides a history of trust in vaccines from a clinician’s perspective. Changing parental expectations include old-style medical paternalism giving way to patient empowerment and choice, increasing popularity of “natural” mothering, and consumerism increasingly being promoted in medicine. The result, as described by Dr. Baker, was the perfect storm whereas the “autism epidemic” met vaccine skepticism. Dr. Baker argues that vaccine hesitancy – like autism – is a spectrum whereas a few might fit the stereotype of extreme distrust and conspiracy theories, but far more people find themselves honestly worried. People want to make choices in according to their values which vary tremendously between people. No “one size fits all” is sufficient to address the varying concerns and values that clinicians encounter. Trust in doctors is critically important for patient decision making, particularly around vaccines.
Dr. Baker and the great majority of physicians and public health personnel involved in vaccines and vaccine programs were unaware of the amount of mercury in thimerosal containing vaccines in 1999 when the FDA review revealed that the potential exposure to ethylmercury among infants to be more than the Environmental Protection Agency considered to be safe based on guidelines for exposure to methyl mercury. The guidelines for methyl mercury were based on low level chronic exposure through diet rather than vaccine exposure to ethyl mercury which were bolus exposures through injection. The active efforts to encourage reduction or elimination of thimerosal in vaccines given to infants was necessary as a precautionary measure because of the uncertainties regarding differences in toxicity between ethyl and methyl mercury. Imagine the public backlash that would have occurred if action was not taken to decrease exposure for infants. The loss in public trust in vaccines, government, and the medical profession would have been very large.
Maintaining trust in vaccines, public health authorities, and health care providers will require a multi-faceted effort. We can improve the public’s understanding of science by increasing efforts to teach scientific decision making at all levels of education. Understanding science and how decision are made overcomes the fallacy of “post hoc ergo propter hoc” or “after this, therefore because of this”. The public needs to know more about the science that goes into the development and evaluation of vaccines. Basic information about vaccines and how they benefit individuals and communities should be included in the curriculum for children, beginning in elementary school and continuing through adolescence.
Many vaccines have been developed with support from the National Institutes of Health which uses a rigorous peer review process for funding studies that have contributed to the development of many of the vaccines available today. The Food and Drug Administration (FDA) conducts in-depth reviews of applications for licensure by manufacturers. Clinical trials are required to characterize efficacy and safety, and proof that the benefits outweigh the potential risks. Also, there is an underappreciation for the careful reviews of evidence that goes into decision making recommendations for the use of approved vaccines coordinated by the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices (ACIP), with input from the American Academy of Pediatrics, the American Academy of Family Physicians, the American College of Physicians, and many other professional societies and organizations. Anyone can now observe these decision making processes by watching the live webcasts of the FDA advisory committee meetings and the ACIP. After licensure the FDA and the CDC monitor vaccines for safety (3).
Fortunately, only 1-2% of parents in the United States are ideologically opposed to vaccines. However, 7 in 10 parents express concerns about the safety of vaccines and 1 of 3 parents express concerns about autism, vaccine ingredients or the number of vaccines given at one visit or the first two months of life(4). Realizing the full potential of vaccines to prevent disability and save lives requires ensuring that this substantial group of concerned, but not ideologically opposed, parents accept timely vaccination for their children. It will require a continuing effort on the part of scientists, clinicians and public health authorities to maintain trust in vaccines to effectively control and possibly eradicate vaccine preventable diseases.
- Centers for Disease Control and Prevention https://www.cdc.gov/measles/cases-outbreaks.html
- World Health Organization: http://www.euro.who.int/en/media-centre/sections/press-releases/2019/measles-in-europe-record-number-of-both-sick-and-immunized
- Department of Health and Human Services. https://www.hsdl.org/?view&did=6793
- Kennedy A, Lavail K, Nowak G, Basket M, Landry S. Confidence about vaccines in the United States: understanding parents perceptions. Health Aff. 2011 Jun; 30(6): 1151-9.
Insights from the Collections
The Consortium's collections provide many opportunities to learn more about the history of vaccinations and public perceptions of science.
Our cross-institutional search tool allows researchers to investigate materials across multiple institutions from a single interface. With more than 4.4 million catalog records of rare books and manuscripts, the Consortium's search hub offers scholars and the public the ability to identify and locate relevant materials.
Search the Consortium search hub.
Some archival materials related to this topic include:
Maurice Hilleman Vaccinology collection, American Philosophical Society Library
Poliomyelitis Records, American Philosophical Society Library
Albert B. Sabin papers, Rockefeller Archive Center
Evidences of the Utility of Vaccine Innoculation: Intended for the Information of Parents (1801), Huntington Library
Report on vaccine virus and on the results of vaccination in the public schools of St. Louis, 1912, Huntington Library
Edward Miller papers, Columbia University Libraries
Vaccination Tracts: Preface and Supplement (1879), The Library Company of Philadelphia
Lyman Spalding Papers, Harvard Library
Dorothy M. Horstmann papers, Yale University Library
Pasteur Vaccine Company ephemera, College of Physicians of Philadelphia
The History of Vaccines: An Educational Resource by the College of Physicians of Philadelphia
Related publications from our speakers:
Vaccine Nation: America's Changing Relationship with Immunization, by Elena Conis; Chicago, 2016
Vaccines, Pesticides, and Narratives of Exposure and Evidence
Vaccination Resistance in Historical Perspective
A Mother's Responsibility: Women, Medicine, and the Rise of Contemporary Vaccine Skepticism in the United States
The Machine in the Nursery: Incubator Technology and the Origins of Newborn Intensive Care, by Jeffrey P. Baker, 1996
History Lesson: Vaccine Trials in the Classroom
Eugenics and the Origins of Autism
Autism at 70--redrawing the boundaries
The first measles vaccine
See also recent work from our fellows:
Road to Eradication: Global Polio Vaccine Testing in the Cold War, Dora Vargha
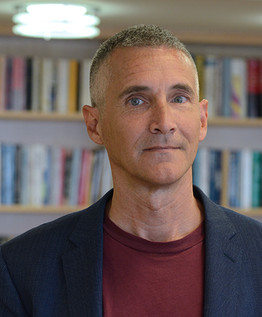




Jeffrey Baker is Professor of Pediatrics and History, and directs the Trent Center for Bioethics, Humanities, and History of Medicine at Duke University School of Medicine. He is a general pediatrician with a focus on children with autism spectrum disorders, and a medical historian whose work has addressed vaccine controversies, autism, and the history of pediatrics.